WHAT IS IT? AND WHAT CAN I DO ABOUT IT?
OVERVIEW
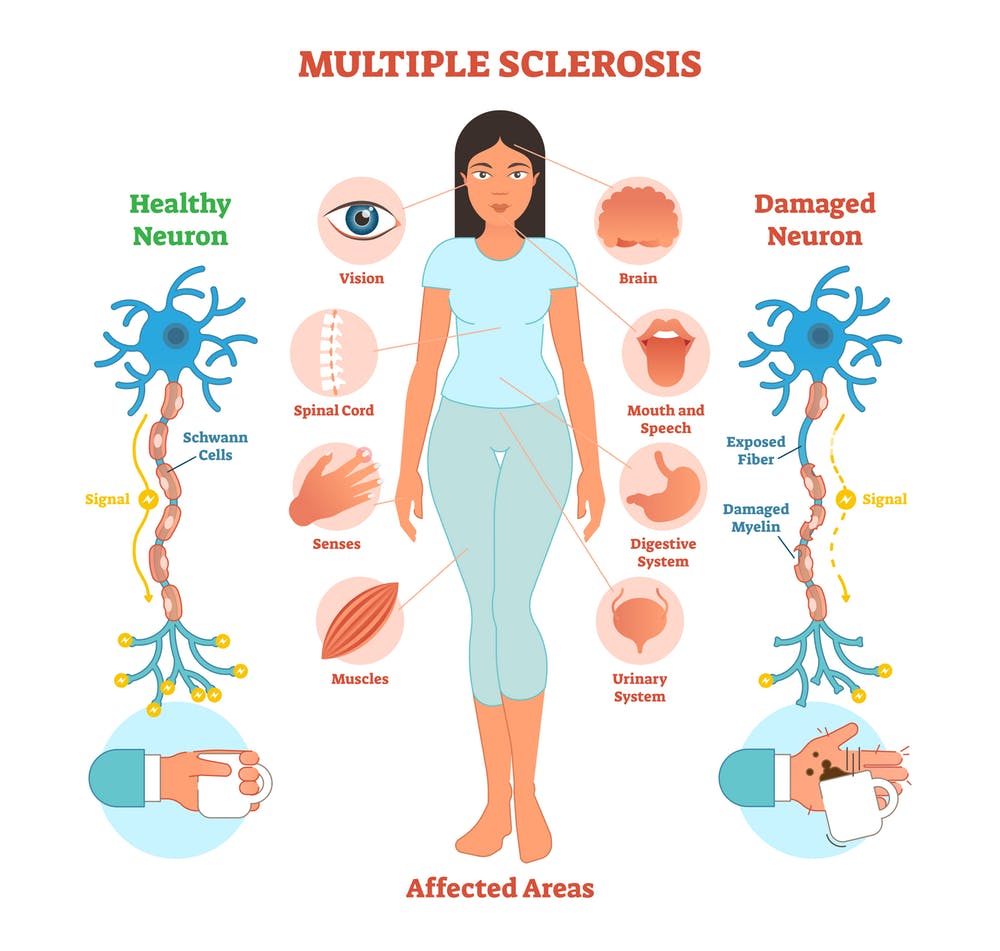
Multiple Sclerosis (MS) is a progressive disease of the Central Nervous System (CNS). It is considered an autoimmune disease that is characterised by a chronic inflammatory response on the myelin sheaths of our CNS. Eventually the myelin is destroyed and the axons of the nerve cells are exposed to attacks from our immune system. The exact cause of MS is unknown but it’s thought to be multi-factorial; Genetic predisposition, environmental exposure to toxic agents, vitamin deficiencies and smoking to name a few. Other Risk factors include;
Age; Typically affects people in the early 20’s - early 50’s
Gender; Women are more than 2 times likely to get MS than Men
Race, climate and having other autoimmune diseases such as Psoriasis and Type 1 Diabetes
Myelin is fatty tissue that surrounds the conducting part of a neuron called the ‘Axon’. Myelin protects the neuron and acts as an insulator to prevent ‘Ion (electrical current) leakage’. As the myelin gets damaged, we have ions leaking along the axon and therefore the signal to the muscle is either much slower, weaker or doesn’t even make it. Because MS can attack any neuron’s myelin in the brain or spinal cord, we have a very wide range of symptoms depending on the lesion site. People with MS can experience physical, cognitive and emotional impairments. There are 4 sub-types of MS and diagnosing which type is important for prognosis and deciding which type of treatment will be most effective.
Relapse Remitting MS (RRMS); Accounts for about 85% of people with MS. It’s characterised by unpredictable acute attacks followed by periods of remission. Remission times can last from weeks to years and functional recovery during remission can range from partial to full.
Primary Progressive MS (PPMS); Accounts for about 10% of people with MS. This type largely affects nerves of the spinal cord. There are little or no remission or acute attack periods as the disease gradually gets worse over time.
Secondary Progressive MS (SPMS); 60 - 70% of people with RRMS will eventually develop SPMS after about 10 - 20 years from diagnosis. However, every case is different and people can move into this stage in a shorter or longer time period. Rate of progression in this stage also varies between people as symptoms gradually get worse overtime without new relapses. It’s thought that after moving into SPMS that nerve damage changes to less inflammation and more so a slow down of how well the nerve functions.
Progressive Relapse Remitting MS (PRMS); Accounts for about 5% of people with MS. Typically associated with symptoms of eye pain, autonomic dysfunction and depression. In this type, there are acute attacks followed by gradual worsening of symptoms instead of remission. Relapse attacks are due to inflammatory attacks and progression of symptoms is due to nerve damage or loss.
TREATMENT
There is no known cure for MS, however there is treatment to slow the progression of the disease and partial symptomatic alleviation. Treatments include Disease Modifying Drugs, Exercise and Diet.
Disease Modifying Drugs;
Because most of the immune response occurs in the early stages of the disease, early and aggressive treatment with these medications can reduce the amount of relapses and slow the formation of new lesions. As this is an autoimmune disease, most of the drugs are immunosuppressants or immunomodulatory and can carry significant health risks. It is essential that you talk through all your treatment options with your neurologist. The majority of disease modifying therapies are for RRMS and they can be takes as injections, orally or as infusions. Corticosteroids are used to treat MS flare ups or attacks and are typically taken in courses of 5 days. There is also currently a lot of research looking at stem cell therapy as a treatment for MS, however, more research is human clinical populations is needed.
Exercise and Physical Therapy
This segment has the potential to be a whole book in its self, therefore I will leave more detailed information for future separate blogs. As you now know, MS has a wide range of symptoms from weakness, impaired gait, fatigue, impaired balance, reduced dexterity, vertigo, memory and executive function loss, depression and the list goes on. These are all impairments due to specific lesion sites in the brain and/or spinal cord. Physical therapy will assess for these impairments and provide exercises to improve strength, walking capacity, balance and other motor symptoms. It will also be important for your therapist to look at assistive technology and mobility aids that would be required at different stages of your disease to ensure you can keep living as independent as possible.
Appropriate exercise programs need to consider modality, dosage, safety and environment. Safety in terms of falls risk and infections, environment in terms of temperature control (MS patients are susceptible to increase in symptoms in too warm or to cold environments), dosage in terms of efficacy and fatigue management, modality in terms client goals and treatment plan. Exercise has also been shown to improve non motor symptoms such as fatigue, cognition, depression and anxiety.
Treating the symptoms is important, but I would argue more importantly exercise should be viewed as a medicine that can help treat the disease head on, being proactive instead of reactive and only treating symptoms. There is no evidence that exercise will cure MS but there is evidence that exercise can slow the progression of MS. Aerobic exercise has been shown to be neuroprotective as it enhances neuroplasticity (repair and restructure of our nervous system) by increasing levels of neurotrophic factors such as BNDF, NGF, NT-3 and IGF-1. These neurotrophins are responsible for repair and regrowth of synapses, blood vessels and neurons in our nervous system. Repeated practice of a skill or functional task as part of therapy results in the brain improving the efficiency of existing pathways or the brain can find existing pathways that are dormant and learn to create the movement or function. Exercise has also been shown to reduce inflammation by reducing pro-inflammatory markers and increasing anti-inflammatory markers. More specific to MS, Oligodendrocytes are the cells in the nervous system responsible for repair and regrowth of Myelin sheaths. Emerging research is showing that aerobic exercise influences oligodendrocyte proliferation and repopulation. Resistance exercise improves neural connections to the muscle and that is actually where our strength gains initially occur. There is research showing that resistance exercise improves perceived fatigue levels in MS, this is likely due to the improved neural efficiency and therefore results in less central (nervous system) fatigue.
Overall, just like a drug has a dose response for efficacy, so does exercise. The current guidelines for people with mild to moderate MS are 30 min of moderate intensity aerobic exercise twice a week and resistance training for major muscle groups twice a week. In terms of promoting neuroplasticity, higher intensity aerobic exercise, skill acquisition and resistance exercise is superior than the current guidelines. Greater the dosage and frequency (i.e. more attentive repetition and goal orientated) is also superior. Keep in mind that the current guidelines are the minimum recommendation, however in MS this needs to be carefully considered as fatigue is a very real and common issue that needs to be addressed on an individual basis when considering dosage.
I hope you have learnt something from this information and it helps direct you to a path of you improving your life. If you would like to learn more or speak to an Exercise Physiologist that specialises in neurological rehabilitation you can reach out to us via our website, Facebook, email or phone. Please click on the ‘contact’ tab for all our information.