WHAT IS HAPPENING? AND CAN IT BE TREATED?
OVERVIEW
Parkinson’s Disease (PD) is a progressive neurodegenerative disease of the brain that affects the control of body movements, cognition and emotion. PD affects 1-2/1000 of the general population with the rate increasing to 1% in people over 60 years old. Diagnosis under the age of 50 is termed 'Young Onset of Parkinson’s Disease (YOPD)’ and is associated with PD genetic risk factors.
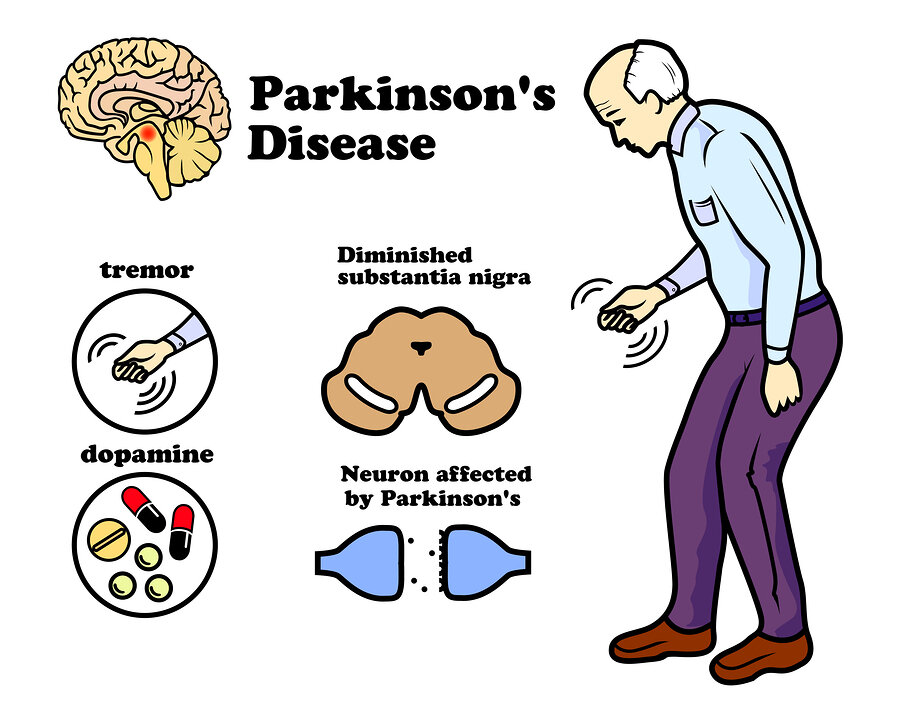
The exact cause of PD is unknown in most cases, with some genetic factors identified in about 10% of patients. It’s becoming increasingly more accepted that environmental factors such as pesticides, toxins and chemical could be contributing to developing PD. Parkinson’s develops as the dopamine producing neurons in the brain begin to die, the region of the brain most affected is the ‘substantia nigra’ within the ‘basal ganglia’. There is a build up of a protein called ‘alpha-synuclein’ forming lewy body plaques in the brain and other cortical regions. As these lewy body plaques spread to other cortical regions, other symptoms and dementia begin to develop. Up to 70% of dopaminergic neurons die before early clinical motor symptoms develop and diagnosis is made. Communication between neurons in the basal ganglia is required for smooth, controlled voluntary movement. In PD, there is damage in this region and this is why we see motor symptoms of tremor, slow movement, rigidity, impaired balance and initiating movement (freezing). Parkinsonism is an umbrella term that covers several conditions with similar symptoms of slow and shuffled movement, rigidity, gait and balance impairments with freezing. They can be referred to as Atypical forms of PD and typically progress much quicker.
Idiopathic PD; most common form of Parkinsonism and the one we are talking about today. accounts for approx. 85% of cases.
Multiple Systems Atrophy (MSA), Vascular Parkinson’s, Progressive Supranuclear Palsy (PSP), Lewy Bodies Dementia and Normal Pressure Hydrocephalus (NPH) are some examples of other Parkinsonism diseases.
The Hoehn & Yahr Scale is commonly used to classify progression and stages of PD depending on patient’s symptoms. The scale moves from 1 (minimal or no functional disability) to 5 (wheelchair and bed bound with severe functional disability). Not everyone develops through all these stages and most people will not die from PD it self. Early treatment is critical and most effective in stages 1-3. Treatment can effectively ease symptoms and slow the progression so that it is unlikely to reach stage 5.
BRAAK STAGING
Braak staging refers to the stages of pathogenesis of the disease. In PD, lewy bodies progress in a predictable manner from one brain region to another depending on the progression of the disease. Lewy Bodies are initially found in the Enteric Nervous System (neurons that control the function of the gastrointestinal tract), the medulla and the olfactory bulb. Interestingly, constipation and reduced sense of smell are some of the earliest signs of PD.
SIGNS AND SYMPTOMS
The cardinal signs of PD are tremor, rigidity, bradykinesia (slow movement) and postural instability. Although, PD has common non motor symptoms such as cognitive issues with attention, memory and executive functioning (e.g. managing finances). It is also common to see behavioural issues such as apathy and depression. It is estimated that 50 - 80% will go on to develop dementia. As PD progresses, the risk of falling greatly increases due to shuffled walking, festernating gait and further worsening in postural instability. About 30% of patients will have autonomic dysfunction which will cause issues with blood pressure, bowel movements, breathing and heart rate. As the disease progresses they will have issues with their speech and swallowing and you will notice the voice become weaker and quiet. Altogether, these symptoms have a tremendous impact on their lives and the lives of their family members and carers.
treatment
Currently there is no known cure but treatment can significantly improve symptoms and slow the progression of the disease. A Multi-modal and Multidisciplinary approach is gold standard to achieve optimal outcomes. A combination of medicine, exercise, diet and surgery have proven to be efficacious in treating PD.
Medication; Drug therapy can very effective in treating symptoms, however there is no research showing they slow the progression of the disease. Early diagnosis and the choice of medicine you take early on is critical in how your condition will develop over time. Make sure to talk this through with your neurologist. Common medications include;
Levodopa: Most commonly prescribed. It is the precursor to the neurotransmitter dopamine and once it crosses the blood brain barrier it is converted into dopamine.
Carbidopa: This drug prolongs the life of available dopamine by blocking the metabolism/re-uptake of levodopa from the blood, therefore allowing a greater portion cross the blood brain barrier. Combining carbidopa with levodopa (Sinemet) allows you to take a much lower dosage of levodopa, therefore preventing many side effects of levodopa such as dyskinesia (involuntary rhythmic movements) that is seen with long term use.
Safinamide: Adjunctive medicine for mid-late stage PD who are starting to have shorter ON periods (symptomatic relief) and longer OFF periods (medicine wearing off). This drug allows patients to experience longer ON periods. However, common side effects include drowsiness, nausea, falls and dyskinesia.
Dopamine Agonists: Pramipexole, Rotigotine, Ropinirole. These drugs mimic the shape and size of dopamine and bind to dopamine receptors. most doctors will prescribe these first and then add levodopa if symptoms are not controlled. They are given first because they don’t have the same risk for long terms side effects of dyskinesia. They can however, cause confusion and hallucinations.
Deep Brain Stimulation (DBS); This is the most common surgical treatment for PD. There are other surgical options which are evolving, however it is beyond the scope of this article to discuss them. DBS is reserved for patients who no longer respond to medication in a predictable manner or suffer medicine induced dyskinesia. DBS can be very effective in treating bradykinesia, rigidity and tremor. DBS acts on the midbrain and basal ganglia and it is reversible and adjustable. Therefore, it favoured as the predominant surgical option.
Exercise; Medicine is an essential part of treatment, but it is only exercise that has been shown to slow the progression of the disease. Medicine combined with exercise is key because it allows for symptom control and then be able to train at your optimum level so you can achieve the required intensity and quality of exercise. Exercise will reduce the frequency and extent of dosage increases of levodopa, therefore decreasing the risk of medicine induced side effects such as dyskinesia. Exercise is effective at treating both motor and non motor symptoms of PD. It has been shown to improve bradykinesia, rigidity, postural instability, cognition, depression, pain, sleep and constipation. Exercise will prolong your independent mobility and therefore allow you to stay physically active, ultimately reducing risk of secondary comorbidities such as diabetes and heart disease.
PD patients present with specific contraindication and complications that need to be considered when prescribing an exercise program. PD patients commonly have autonomic dysfunction which results in an irregular cardiovascular response (changes to heart rate, blood pressure and peak oxygen usage) to exercise. PD also presents with mitochondrial dysfunction, organelles in our cells responsible for the manufacture of energy so our cells and body can function. PD affects muscle POWER more so than STRENGTH, so it’s important the exercise program on developing power more so than strength. Although, building strength is also important for other reasons such as improving goal related function tasks, improving bone density or any other patient specific needs.
PD patients will have differing predominant symptoms (i.e. tremor vs bradykinesia vs rigidity) and exercise program will have slightly different focuses depending on the predominant symptoms. It is therefore essential that you consult with an allied health professional who specialises in exercise prescription for neurological conditions so that optimal, individualised exercise program can be prescribed.
The overall principle for exercise prescription in PD is high intensity, large amplitude movements, powerful and accurate movements (with start and finish points). Exercise should be in intervals with frequent rest periods between exercises because of the high intensity required. Low to moderate intensity exercise will be beneficial for general health and well being, improving cardiovascular function etc… but for it to be neuroprotective and promote neuroplasticity in Parkinson’s, it requires large, powerful and high intensity exercise. That’s not to say moderate intensity will not promote neuroplasticity or improve PD, it’s just that higher intensity has been shown to be MORE effective for these desired outcomes. And of course, not everyone will be able to engage in high intensity exercise to begin with so an individualised and graded approach is needed.
It is well established that exercise increases levels of BDNF (brain derived neurotrophic factor) and other neurotrophic factors which are responsible for growth, repair and protection of our neurons and nervous system. Exercise has also been shown to improve attention and memory in patients with mild cognitive impairment via increases to size of a brain region called the ‘hippocampus’ and it is thought that the same effects are seen in PD patients. Therefore, helping delay/prevent dementia in this population group. A combination of aerobic, resistance, mobility, balance and agility training specific to an individual’s symptoms and condition is recommended. Exercise at moderate to high intensity at least twice a week for 60 min a session is a good guideline for the minimum amount of exercise required.
Diet; There is a body of evidence suggesting that a ketogenic diet (high fat - very low carb) can be beneficial for neurological conditions. In a ketogenic diet, the body and brain begin to use ketones as a primary source of fuel instead of glucose. There is some, but limited research suggesting this diet can help Parkinson’s. It also recommended to eat foods high in Omega - 3 and Vitamin D. It is extremely important you speak with your specialist and a dietitian before changing or starting a new diet because certain foods will interact with your medication. Also, the ketogenic diet puts the body into ketosis and will have high levels of ketones in the body, this can result in a severe/deadly condition called ketoacidosis.
Overall, treatment can significantly improve your symptoms and quality of life. A combination of medicine and exercise is the gold standard for treatment. I hope you have learnt something from this information and it helps direct you to a path of you improving your life. If you would like to learn more or speak to an Exercise Physiologist that specialises in neurological rehabilitation you can reach out to us via our website, Facebook, email or phone. Please click on the ‘contact’ tab for all our information.